Wounds in diabetic patients are characterized by a detrimental microenvironment due to vascular pathology, neuropathy, and chronic inflammation, posing significant clinical challenges for healing and functional recovery. Although traditional electrical stimulation can promote cell proliferation and migration, reduce inflammation, and modulate blood circulation to accelerate wound repair, it faces several limitations: rigid metal electrodes that may trigger inflammatory responses and infection, bulky external power devices requiring wired connections, cumbersome operation, and high cost. Additionally, impaired sensory perception in patients makes it difficult to detect hazardous wound conditions, further complicating wound management and increasing the economic burden on care.
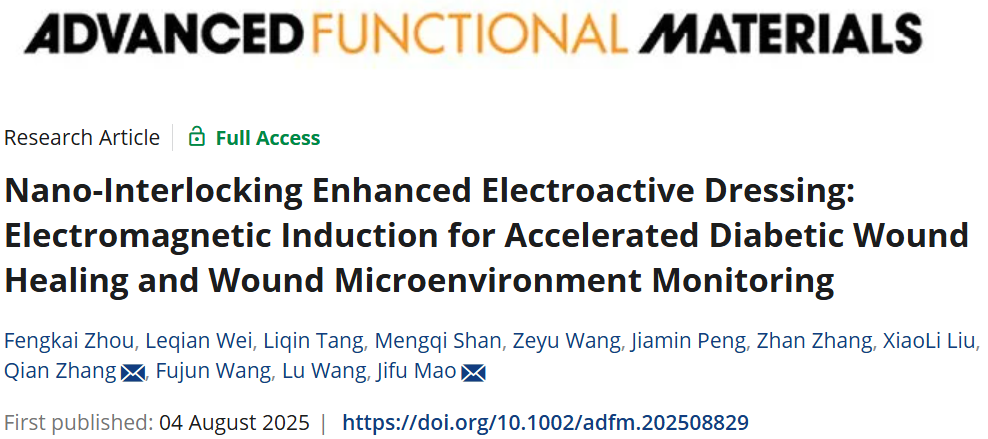
Recently, a research paper titled “Nano-Interlocking Enhanced Electroactive Dressing: Electromagnetic Induction for Accelerated Diabetic Wound Healing and Wound Microenvironment Monitoring” was published online in Advanced Functional Materials, with Researcher Mao Jifu from the College of Textiles and Associate Researcher Zhang Qian from the College of Biological and Medical Engineering at Donghua University serving as co-corresponding authors. The team developed an electromagnetic induction-powered electroactive dressing that enables both wireless electrical stimulation therapy and wound microenvironment monitoring. Through the integration of electrospinning and electrospraying techniques, a nano-interlocking structure was formed between Ti₃C₂Tₓ MXene and polycaprolactone fibers, endowing the dressing with excellent conductivity (≈3.5 S cm⁻¹). Under a rotating magnetic field, the dressing generates a wireless micro-current of 10.8 μA, which activates pro-healing pathways (including calcium signaling, TGF-β, PI3K-AKT, PPAR, axon guidance, and Wnt pathways) while inhibiting inflammatory pathways (such as TNF and NF-κB pathways). This dual modulation of cellular behavior and the immune microenvironment accelerated wound healing by approximately 36.3% and enhanced nerve regeneration by about 283.8% compared to the control group. Furthermore, the dressing can monitor physiological parameters of the wound—such as temperature, strain, and exudate—enabling timely and precise wound care and thereby advancing the fields of electromagnetic induction biomedicine and personalized medicine.
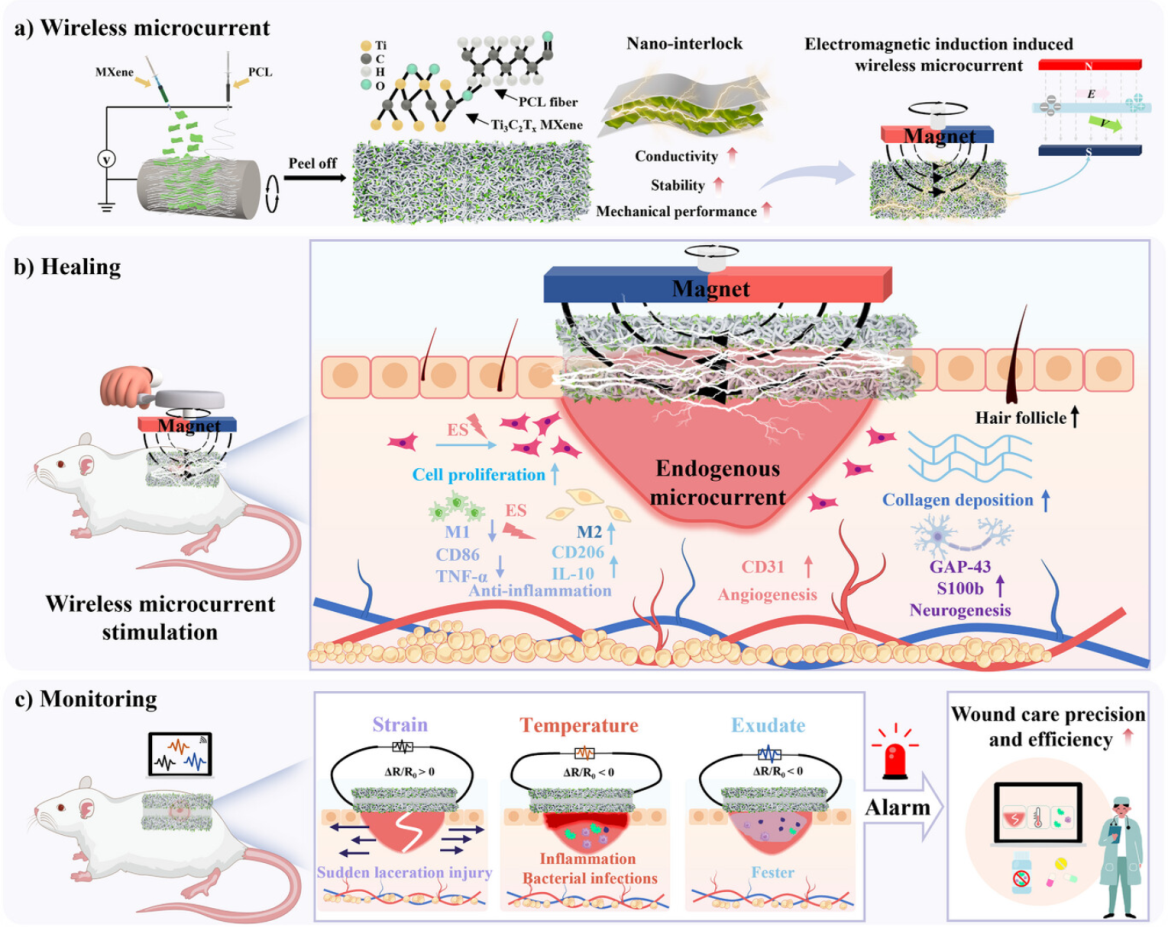
Figure 1 electroactive dressing promotes diabetic wound healing and microenvironment monitoring via electromagnetic induction
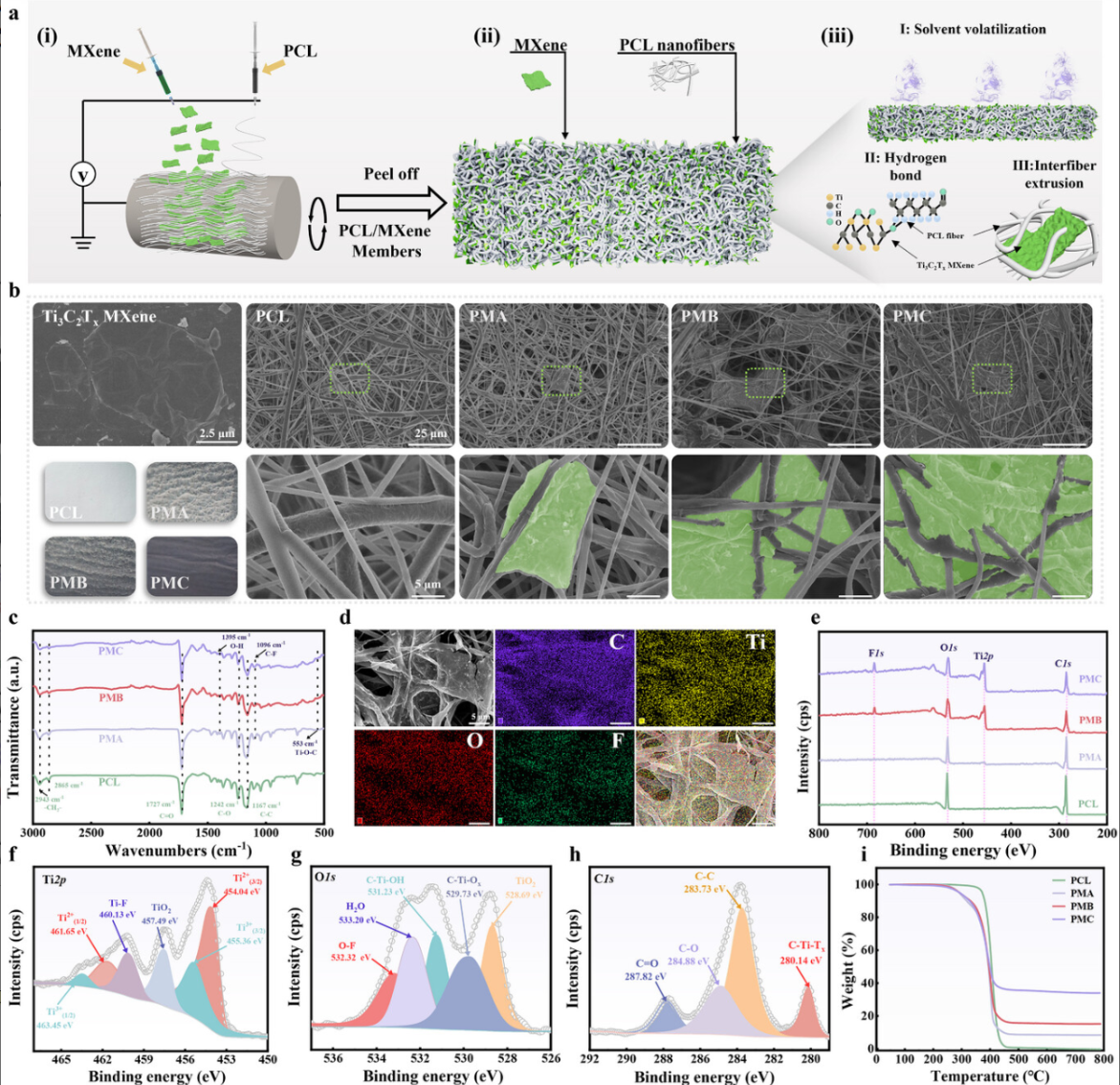
Figure 2 preparation and characterization of the electroactive fibrous membrane
Figure 3 mechanical properties and wireless microcurrent testing of electroactive fiber membranes
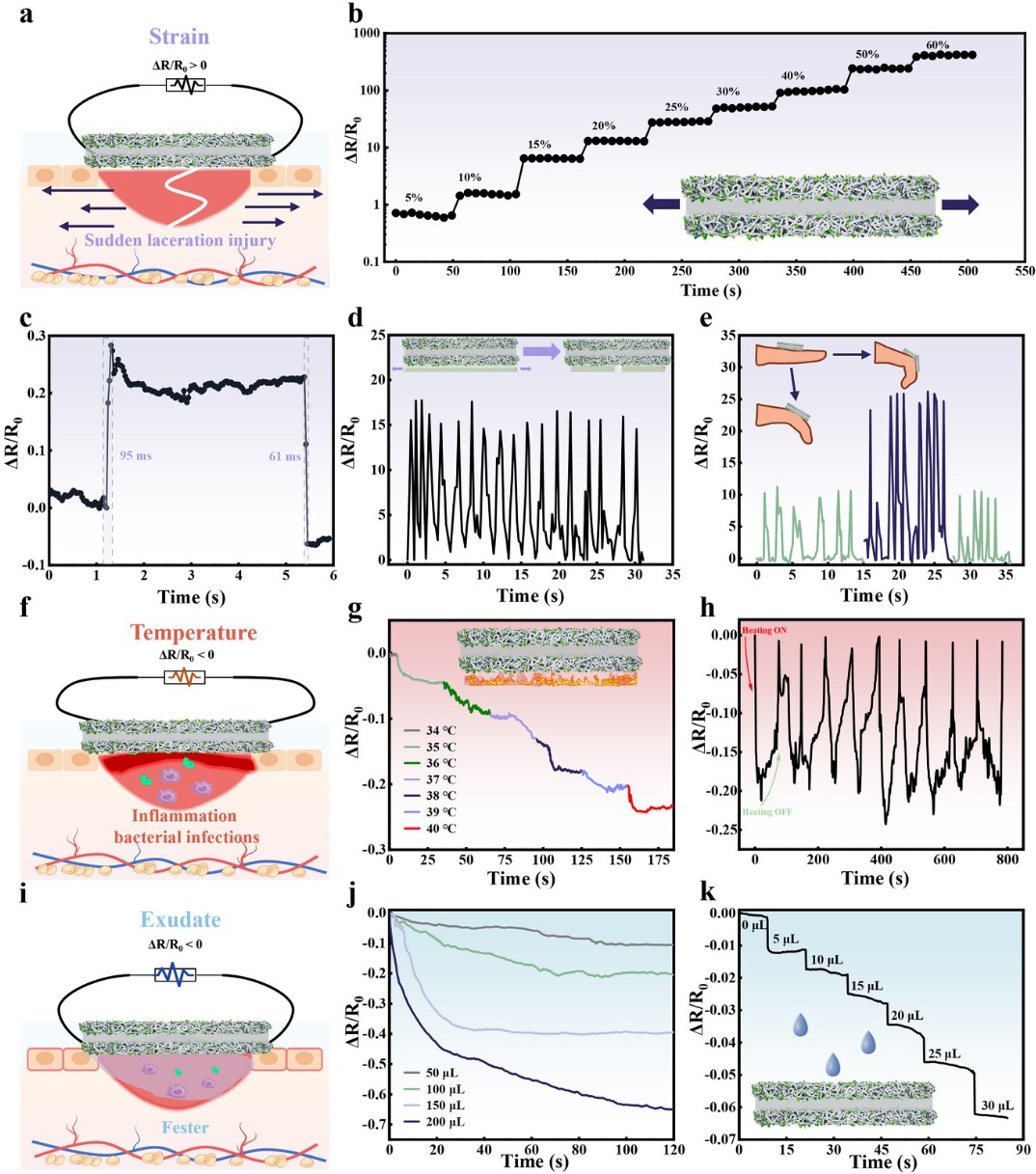
Figure 4 in vitro diagnostic monitoring function of electroactive fiber membranes
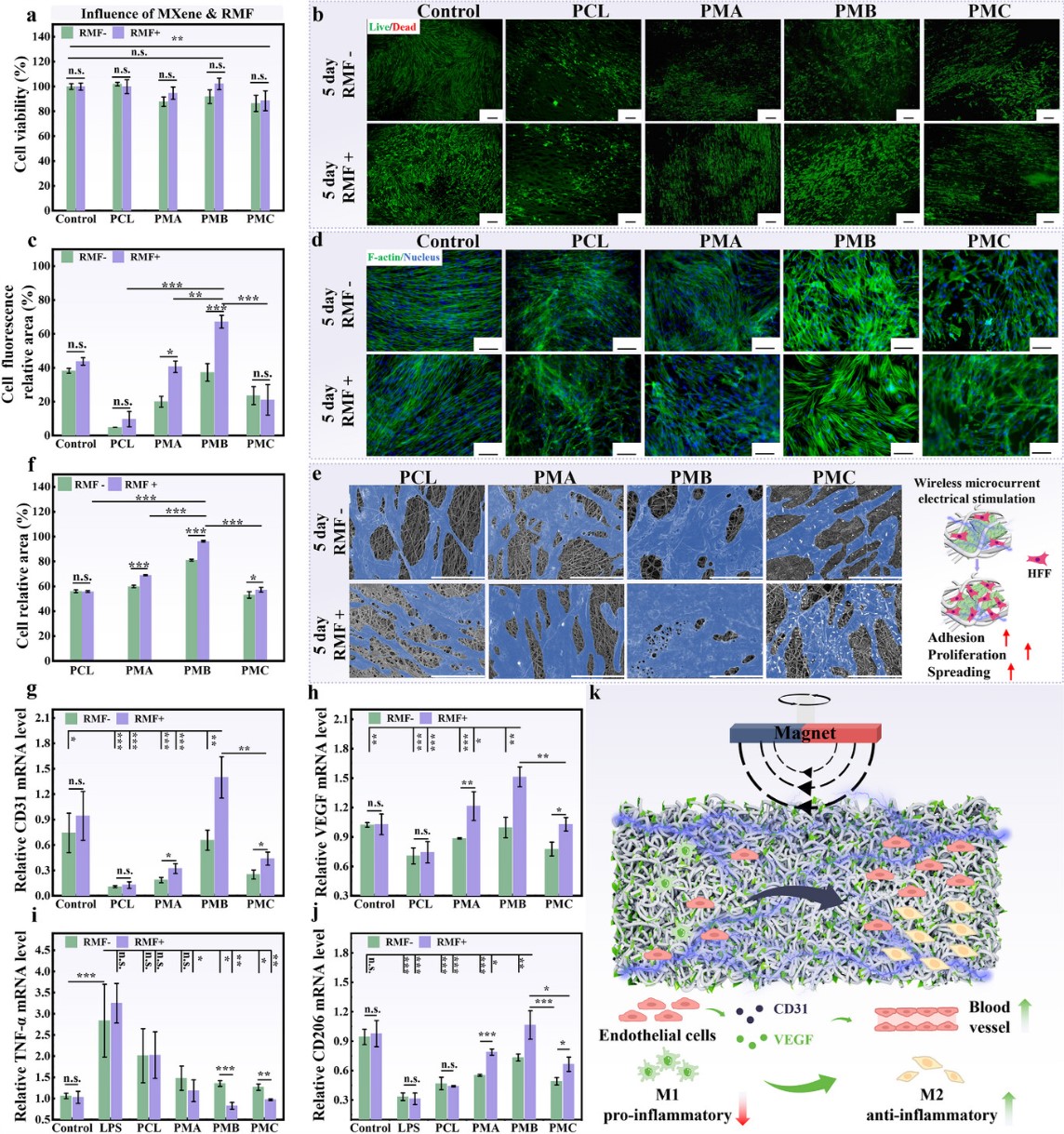
Figure 5 regulation of cell behavior by radio signals generated via electromagnetic induction in electroactive fiber membranes
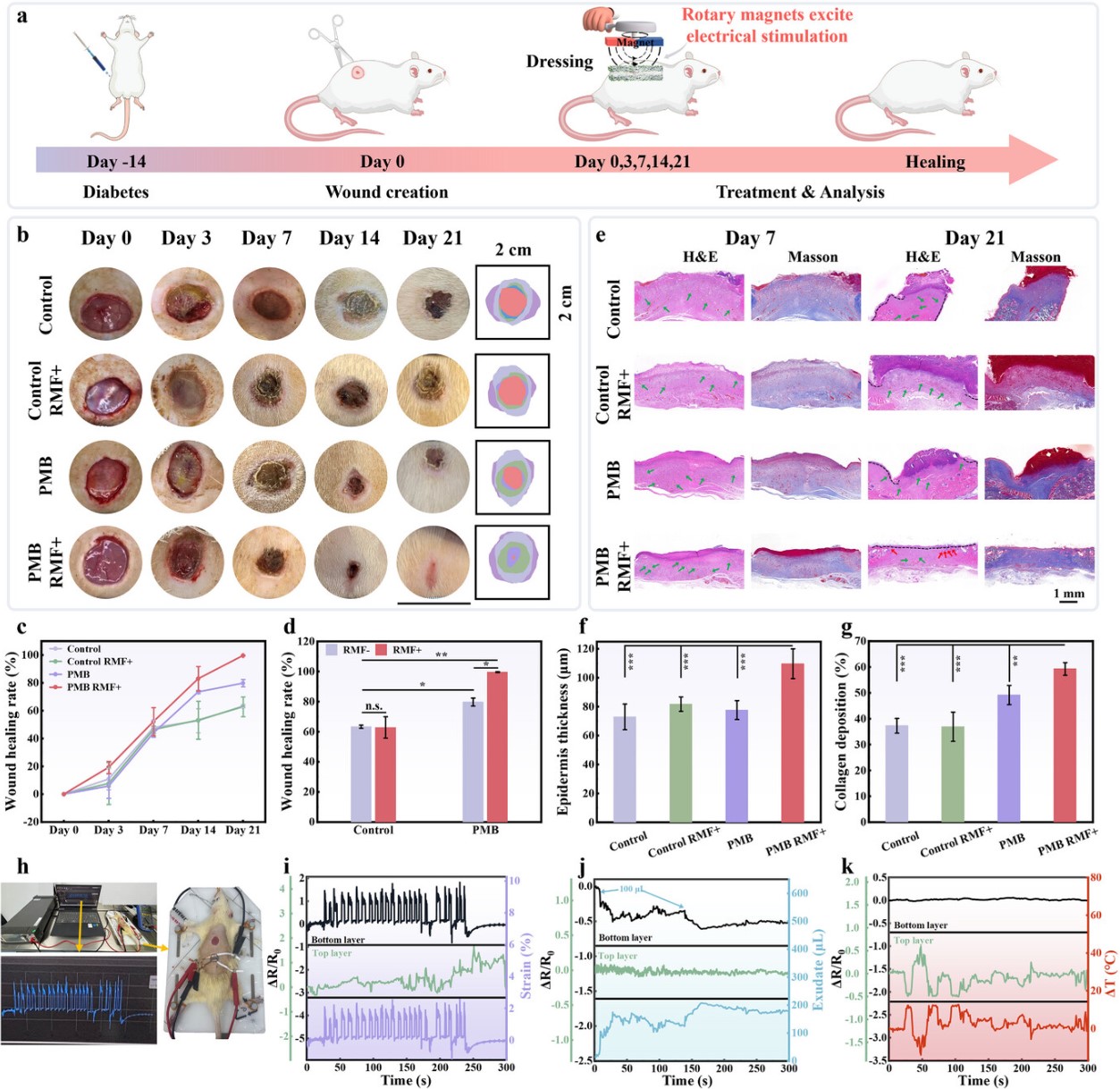
Figure 6 wireless microcurrent based on electromagnetic induction accelerates rapid healing of diabetic wounds
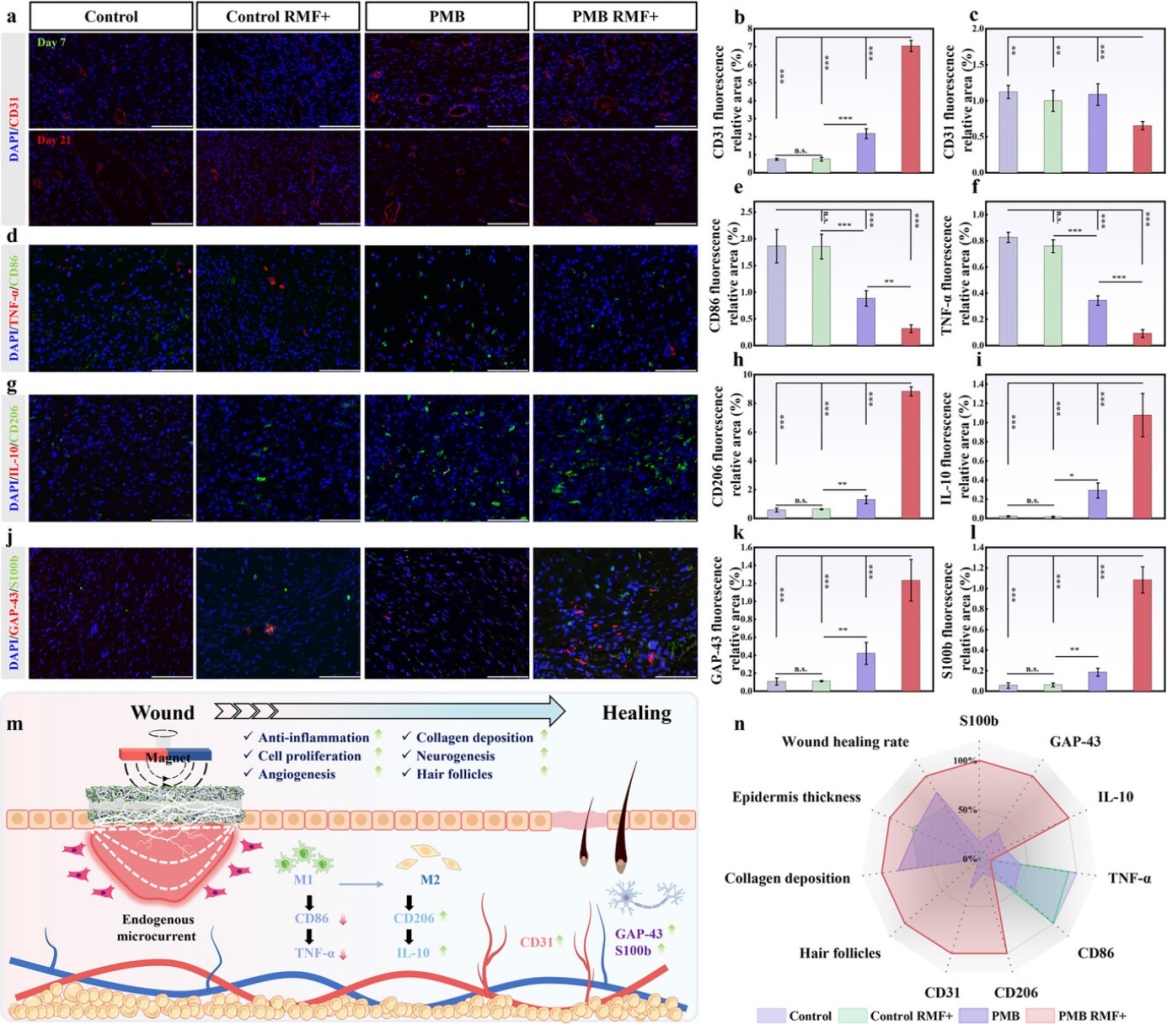
Figure 7 immunofluorescence analysis of wound healing
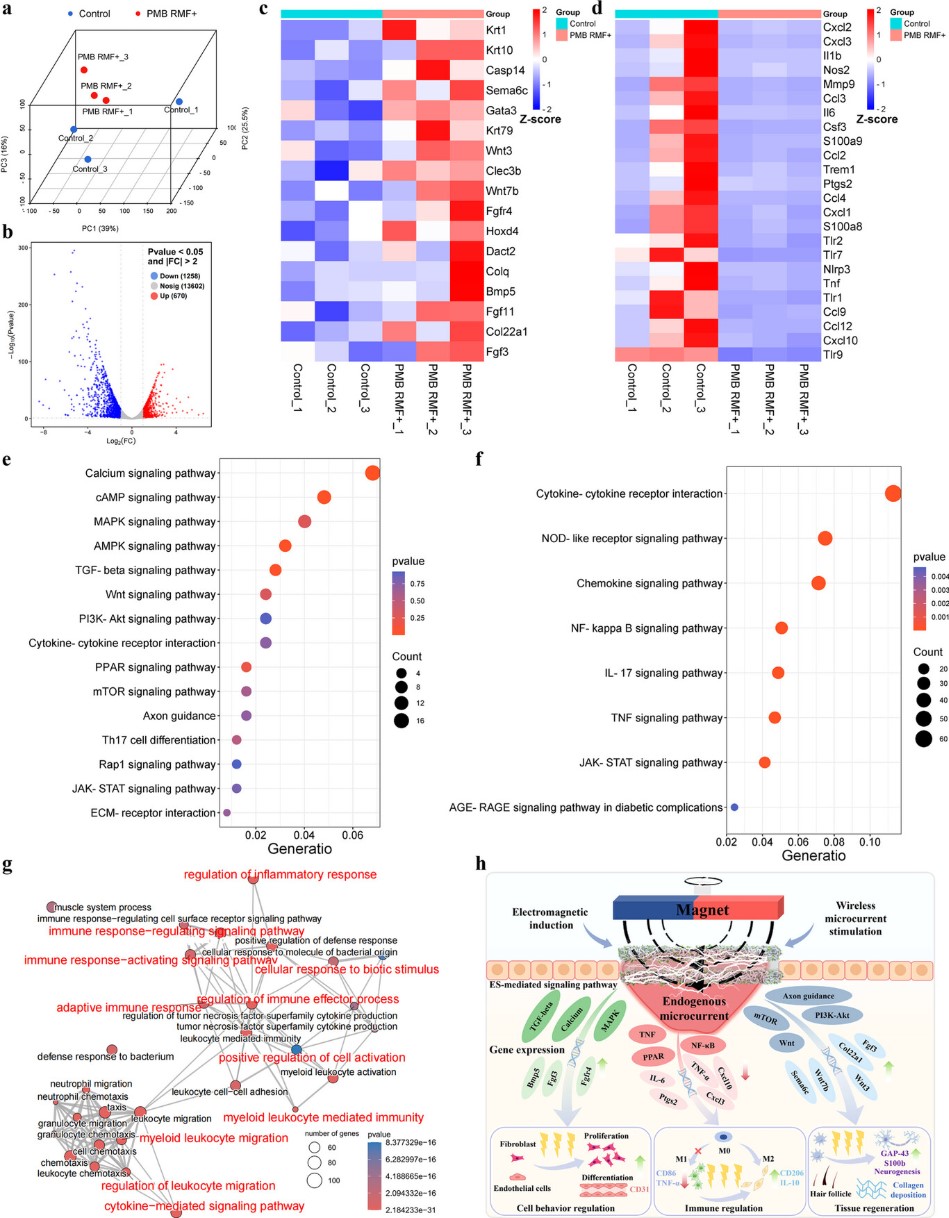
Figure 8 sequence analysis of wound tissue RNA
In this study, a wireless, self-powered electroactive dressing based on electromagnetic induction has been successfully developed, which facilitates rapid healing and functional skin regeneration in diabetic wounds while enabling real-time monitoring of the wound microenvironment. The nano-interlocking structure formed between Ti₃C₂Tₓ MXene and PCL fibers endows the dressing with excellent mechanical properties and high conductivity. In vitro and in vivo studies demonstrate that the wireless micro-current generated by the electroactive fibrous membrane via electromagnetic induction effectively regulates cellular behaviors (proliferation, migration, and differentiation). RNA sequencing results confirm the activation of multiple signaling pathways such as calcium, TGF-β, PI3K-AKT, PPAR, and Wnt, along with the down-regulation of TNF, NF-κB, and IL-17 pathways. These changes modulate gene expression and cytokine release, thereby alleviating inflammation and promoting extracellular matrix remodeling, wound closure, and regeneration of skin appendages including nerves and hair follicles. Furthermore, by utilizing the resistance responsiveness of the electroactive fibrous membrane to temperature, strain, and exudate, the successful monitoring of physiological signals in the wound microenvironment has been achieved, contributing significantly to the advancement of intelligent healthcare toward more precise and efficient wound management. This strategy, characterized by its portability, non-invasiveness, wireless operation, and monitoring capability, highlights its strong potential for clinical application in diabetic wound healing.
Information of this paper:
F. Zhou, L. Wei, L. Tang, M. Shan, Z. Wang, J. Peng, Z. Zhang, X. Liu, Q. Zhang, F. Wang, L. Wang, J. Mao, Nano-Interlocking Enhanced Electroactive Dressing: Electromagnetic Induction for Accelerated Diabetic Wound Healing and Wound Microenvironment Monitoring. Adv. Funct. Mater. 2025, e08829.
Original link to this article: https://doi.org/10.1002/adfm.202508829
